Lower back pain and Sciatica
Anatomy, Pathology & Management
Sciatica accompanies about 10% of lower back pain episodes and nerve root compression by disc herniation is known to be a common cause of sciatica (7).It is estimated that 90% of sciatica cases are the result of a disc herniation or disc bulge in the lumbar spine that compresses on the sciatic nerve root (5).
Symptomatic disc herniation is therefore probably a common presentation in osteopathic clinics. Three categories of disc herniation are generally recognised, consisting of disc protrusions (in which the nuclear material protrudes or bulges against the annulus), extrusions (in which the nuclear material escapes the border of the annulus), and sequestration (when the extruded nuclear material loses contact with the remaining disc nucleus)(7).
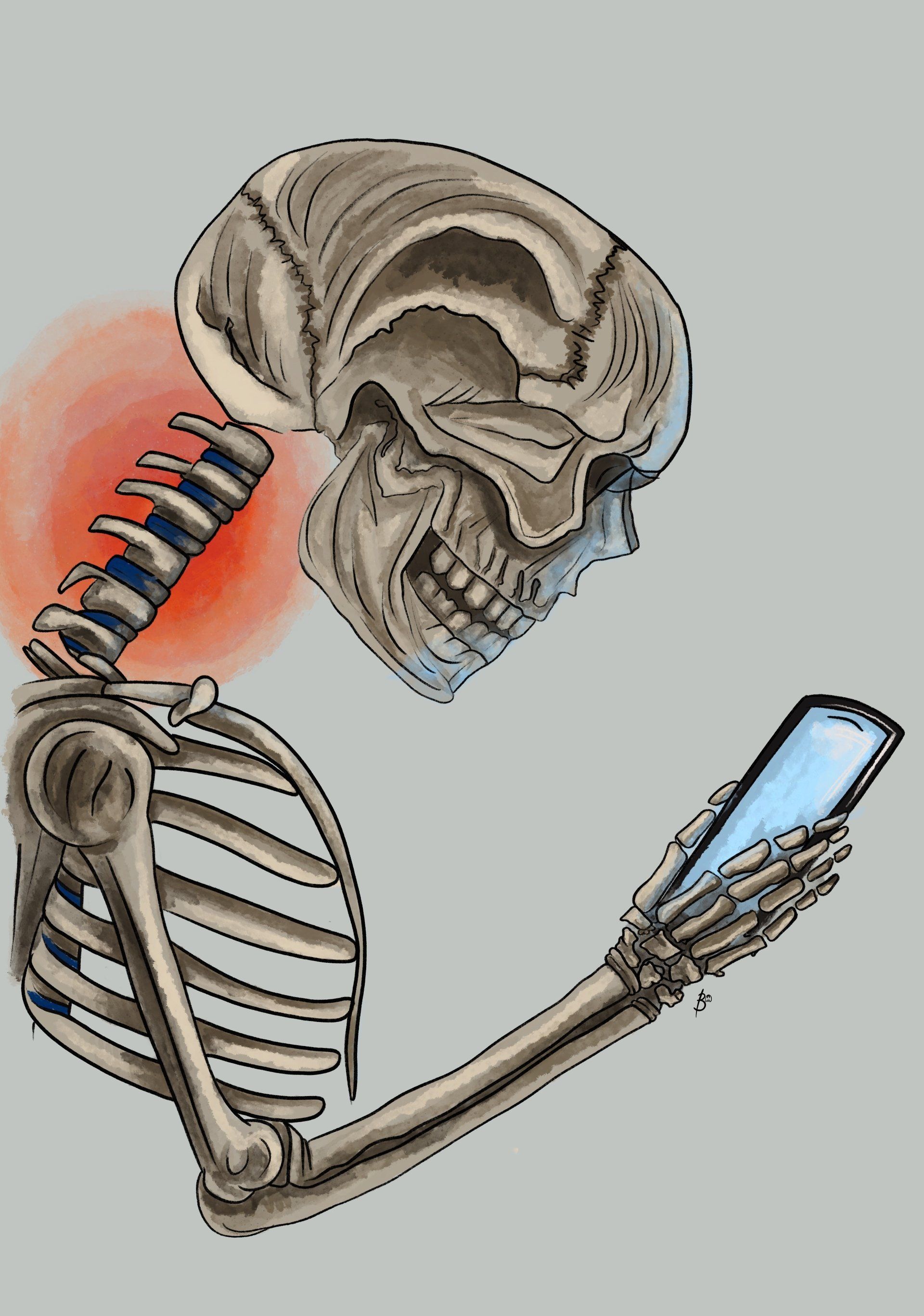
Sciatica is mainly diagnosed via case history taking and physical examination, individuals may be asked to report the distribution of their pain and whether they are experiencing radiation below the knee. Symptoms of sciatica is commonly a radiating shooting pain and/or the experience of numbness or tingling down the back of one or both legs which is also known as radiculopathy (9, 17). It may include the inability to walk depending upon where the pressure of the sciatic nerve occurs(18).
Statistically, approximately 60% of patients visiting primary healthcare with lower back pain (LBP) report back-related leg pain and it is estimated 5%-10% of patients with LBP have sciatica (9). The annual prevalence of intervertebral disc related sciatica in the general population is estimated to be 2.2% of all cases (9).
Anatomy
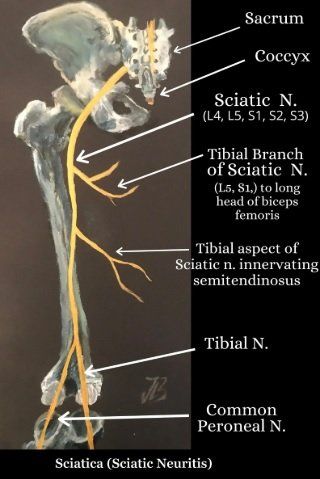
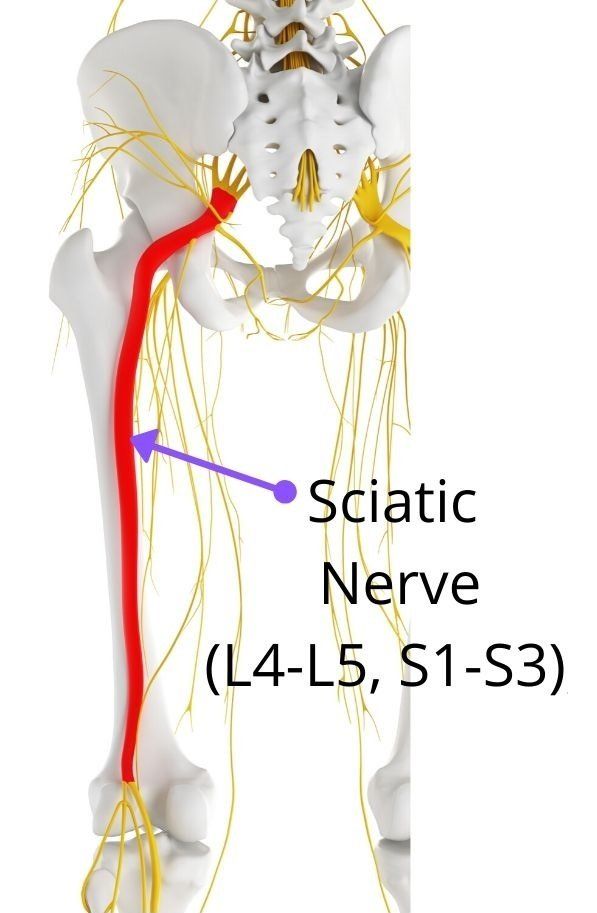
The sciatic nerve (SN) is formed in the pelvis by the joining the ventral rami L4-S3 SN roots (22) (figure 1). It travels inferiorly into the pelvic surface of the coccygeus muscle and enters the gluteal region. The SN leaves the pelvis through the greater sciatic foramen below the piriformis muscle and passes deep to the gluteus maximus
(buttock)
muscle before descending between the greater trochanter and ischial tuberosity in the gluteal region. The trunk of the sciatic nerve innervates the proximal parts of all three hamstrings muscles (semi membranosus, Semi tendonosus and Biceps Femoris) and ischial aspect of the adductor muscles (4).
The sciatic nerve then divides at the apex of the popliteal fossa into two main branches; the tibial nerve
and the common fibular nerve
(figure 1).
After the SN bifurcation, the tibial component innervates the semi membranosus, semi tendinosus, long head of biceps femoris muscles and adductor magnus. The short head of the biceps femoris is innervated via the common peroneal component of the SN.
Risk Factors
Men Vs Women
Self-reported lumbar radicular pain is more prevalent among women (25), and they seem to experience slower recovery from
severe sciatica (54), while men have a higher incidence of hospitalization and surgery due to sciatica.
Obesity
Obesity may slow down the healing of a disc injury and interfere with the nutrition of the intervertebral discs, leading to an impaired healing process. Carrying excess weight may also contribute to the development of chronic, low-grade inflammation within the spine through the release of inflammatory mediators from excess adipose tissue. Obesity-related chronic inflammation may lead to the development of sciatica or the persistence of sciatica symptoms. In a 3-year follow-up study of sciatica patients, BMI was the strongest predictor of incident lumbar artery occlusion, which also suggests that impairment of nutrition can be one of the pathways of obesity’s relationship with sciatica.
Common Symptoms
- Unilateral leg pain is greater than lower back pain (9).
- Radiated pain below the knee into the foot or toes with either numbness or paraesthesia in the same distribution (radiculopathy symptoms).
- Referred leg pain not related to a nerve root pathology (10).
- Radiated pain with a dermatomal pattern.
- Lower back pain.
Common Causes
- Herniated Intervertebral Disc: Herniated lumbar disc is a displacement of disc material (nucleus pulposus or annulus fibrosis) beyond the intervertebral disc space (8).
- Sciatic Nerve Entrapment: May occur from the pelvis to the distal thigh. The most common site is between the greater sciatic notch and ischial tuberosity and by the piriformis muscle. Myositis ossificans (bone tissue formation inside muscle) of the biceps femoris muscle is another possible site. Biceps femoris muscle insertion on the linea aspera to the adductor magnus muscle is also another possible entrapment site to compress the sciatic nerve (14).
- Piriformis Syndrome: The entrapment of sciatic nerve as it exits the greater sciatic notch islikely due to a myospasm or contracture of muscles i.e. piriformis or gemellus superior muscle (4).
- Lumbar Spinal Stenosis (LSS): The anatomical narrowing of the spinal canal which can be associated with various clinical signs and symptoms including back pain and claudication (19). Patients frequently complain of numbness and pain within the lumbar region and lower limbs along with intermittent neurogenic claudication caused by compression of the nerve roots with narrowing of the spinal canal and the intervertebral foramen which can lead to gait disorders (11).
Conditions Related to An Injured Sciatic Nerve
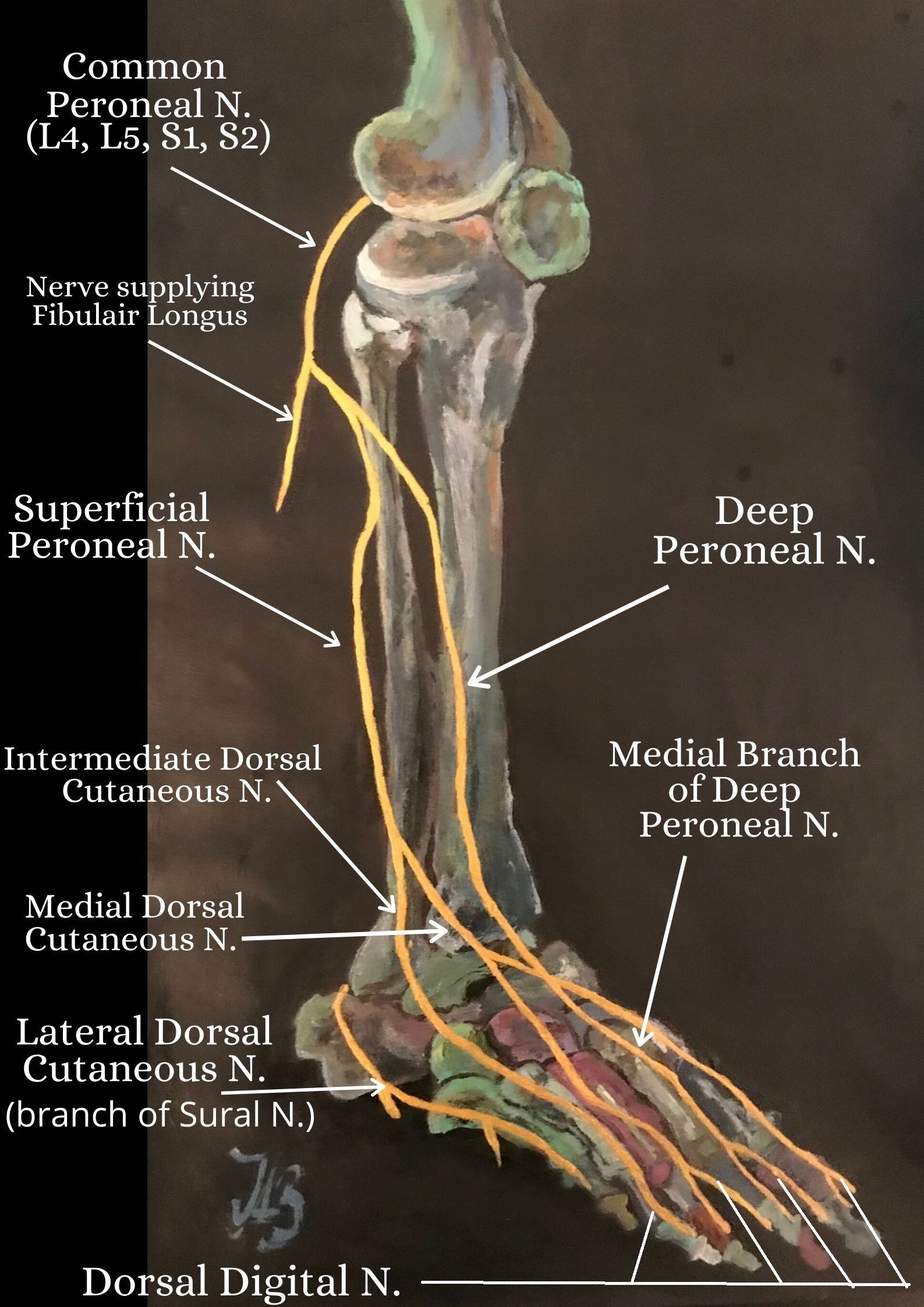
Injury to the Deep Fibular Nerve
An isolated lesion of the deep fibular nerve can lead to muscular innervation being affected and cause the prevention of dorsiflexion resulting in foot drop and a steppage gait (4).
A steppage gait is a gait abnormality that is often adopted to counteract the effects of foot drop by exaggerating the flexion at the hip and knee during walking to allow the toes to clear the ground.
The tibial nerve then passes through the tarsal tunnel of the medial ankle and divides into two terminal branches; the medial plantar nerve and the lateral plantar nerve. These two terminal branches of the tibial nerve supply all the muscles on the plantar aspect of the foot (4).
Tarsal Tunnel Syndrome
Compression of the tibial nerve or either of its terminal branches (lateral or medial plantar nerve) in the tarsal tunnel leads to a condition known as tarsal tunnel syndrome. A patient with the syndrome may experience plantar pain and sensory disturbances and can also result in palsies of the intrinsic foot muscles (4).
Injury to the Common Fibular Nerve
The sciatic nerve is the most commonly injured nerve in the lower limb and because of its subcutaneous position around the head of the fibula, it is vulnerable to direct trauma (17, 4).
Damage to the common fibular nerve at the neck of the fibula can cause weakness or paralysis of the muscles in the anterior and lateral compartments of the lower limb. This can cause a loss of dorsiflexion which often results in foot drop.
Foot drop
Foot drop is a type of gait abnormality in which the toes cannot clear the ground during walking. If damage to the common fibular nerve occurs after it divides into its terminal branches, symptoms are dependent at which the terminal branches have been affected. For example, an isolated lesion of the superficial fibular nerve generally affects sensory innervation which can cause pain in the distal leg and the dorsum of the foot (4).
Treatment

The primary aim of conservative treatment for sciatica from a physical therapist is to reduce the pain and reduce the pressure on the sciatic nerve root. Initially, intervention for the treatment of patients with sciatica is a nonoperative approach which has demonstrated to be beneficial in more than 50% of patients (13).
Corticosteroid Injections
Epidural corticosteroids administered locally
at the site of a lesion has a higher tendency to be effective during the
first weeks of an episode of sciatica.Compared to no epidural corticosteroid administration, epidural corticosteroids may be more effective at improving limb pain at
2 weeks, but may be no more effective after more than 2 weeks in people with disc herniation (8).
Surgery
Surgical intervention is often considered for if symptoms persist for more than 8 to 12 weeks and is generally regarded as the "last resort" in many cases after a very long journey through failed medical management (13). Surgical intervention for sciatica focuses on removing the disc herniation via the removal of part of the disc or foraminal stenosis and is the choice for unilateral sciatica. The aim of the treatment modality is to ease the leg pain, but the predominantly focuses on reducing or removing lower back pain (9). Cauda equina syndrome is an indication for the need for immediate surgery.
Surgical intervention has been compared to conservative treatment for patients with sciatica. Koe et al.,
(2009) found that surgical intervention may provide a quicker relief of symptoms after one year and gain quicker relief of leg symptoms than patients receiving conservative treatment. But, no significant differences were found in terms of success rate in one or two years time during the patients' follow up, in some cases after 4 and 10 years follow up (9).
From a therapist's perspective, the success rate and outcome may vary from one individual to another and factors that need to be considered is the patient's severity of their present condition, lifestyle, previous exercise history and whether they have any underlying conditions which may or may not have been diagnosed whilst having consulted a practitioner. Patient preference for treatment modalities and methods will also differ.
Both standard discectomy
and microdiscectomy
seem to increase self-reported improvement to a similar extent(8).
Conservative Management
Additional options include careful use of anti-inflammatory medications, physiotherapy, massage therapy, local injections, acupuncture and chiropractic treatment. There is no clear medical or scientific evidence as to whether particular interventions do help sciatica or lumbar disc herniation. From my clinical experiene, patient education is of paramount importance with encouraging clients to understand how to manage their injury. Recovery rates are unique and individual for everybody as lifestyle factors, exercise history, body biomechanics and posture all play pinnacle roles.
For example, a 47 year old gentleman, Bill sits working at a computer desktop for 9 hours, 5 days a week. His diet consists mainly of convenience foods high in processed fats and salts, performs less than 2 hours of weekly exercise by walking to work from his car and back at the end of a long day. His recovery rate is predicted to be slower than 29 year old Andrew who is a full time postman, has an active lifestyle, has healthy diet and has attended a gym four times a week for the past ten years and plays a sport.
Spinal Manipulation
Spinal manipulation for sciatica has been found to help improve patient outcomes, some studies have found by up to 50%(13).
References
- Adibatti, M., V. S. (2014) Study on Variant Anatomy of Sciatic Nerve, Journal of Clinical and Diagnostic Research , 8; 8: 7-9.
- Anbumani, T. L., Thamarai Selvi, A., Anthony Ammal S. (2015) Sciatic nerve and its variations: an anatomical study. Int J Anat Res.;3 (2): 1121–1127.
- Bueno-Gracia, E., Estébanez-de-Miguel, E., López-de-Celis, C., Shacklock, M., Caudevilla-Polo, S., González-Rueda, V., Pérez-Bellmunt, A. (2020) Effect of ankle dorsiflexion on displacement and strain in the tibial nerveand biceps femoris muscle at the posterior knee during the straight leg raise:Investigation of specificity of nerve movement,
- Crumbie, L. (2019) [online] Sciatic Nerve: Kenhub.com , last viewed 31/05/2020; www.kenhub.com /en/start/anatomy-sciaticnerve-branches.
- Frost, L. R., Brown, S. H. M. (2016) Muscle Activation Timing and Balance Response in Chronic Lower Back Pain Patients with Associated Radiculopathy, 32; 124-130.
- Gilroy, A. M., Macpherson, B. R., Ross, L. M. (2008) Atlas of Anatomy, Thieme, New York.
- Green, B. N., Johnson, C. D., Snodgrass, J., Smith, M., Dunn, A. S. (2016) Association Between Smoking and Back Pain in A Cross-Section of Adult Americans, Cureus, 8; 9: 1-10.
- Inman, J., Thomson, J. P. (2019) Complementing or Conflicting? A Qualitative Study of Osteopaths’ Perceptions of NICE Low Back Pain and Sciatica Guidelines in the UK, IJOM, 31: 7–148.
- Jordan, J., Konstantinou, K., O'Dowd, J. (2009) Herniated Lumbar Disc, Clinical Evidence, 03; 1118: 1-33.
- Koes, B. W., Tulder, M. W., Peul, W.C. (2007) Diagnosis and Treatment of Sciatica; Clinical Review , 334: 1313-1317.
- Konstantinou, K., Dunn, K. M., Ogollah, R., Lewis, M., Windt, D. v. d., Hay, E. M. (2018) Prognosis of Sciatica and Back-Related Leg Pain in Primary Care: the ATLAS Cohort, The Spine Journal, 18: 1030-1040.
- Kuwahara, W., Deie, M., Fujita, N., Tanaka, N., Nakanishi, K., Sunagawa, T., Asaeda, M., Nakamura, H., Kono, Y., Ochi, M. (2016) Characteristics of Thoracic and LUmbar Movements During Gait in Lumbar Spine Stenosis Patients Before and After Decompression Surgery, Clinical Biomechanics, 5: 15-19.
- Lakshmi, R., Pharm, A. (2018) A Review of Etiology Pathogenesis, Treatment of Sciatica
, JJSR, 7;1: 1477-1479.
- Lewis, S., Jurak, J., Lee, C., Lewis, R., Gest, T. (2016) Anatomical variations of the sciatic nerve, in relation to the piriformis muscle, Translational Research in Anatomy,
- McMorland, G., Suter, E., Casha, S., du Plessis, S.,Hurlbert, R. J. (2010) Manipulation or Microdiskectomy for Sciatica? A Prospective Ranomised Clinical Study, Journal of Manipulative and Physiological Therapeutics, 33; 8: 576-584.
- Monteleone G, Stevanato G. Entrapment of the sciatic nerve at the linea aspera: A case report and literature review. Surg Neurol Int 19-Oct-2016;7:89. Available from: https://surgicalneurologyint.com/surgicalint-articles/entrapment-of-the-sciatic-nerve-at-the-linea-aspera-a-case-report-and-literature-review/
- Netter, F. H. (2014) Atlas of Human Anatomy: 6th Ed., Elseiver Saunders, USA.
- NICE guideline (2016) [ONLINE] Low back pain and sciatica in over 16s: assessment and management, https://www.nice.org.uk/guidance/ng59/ifp/chapter/What-are-low-back-pain-and-sciatica , last viewed 28/05/2020.
- Palastanga, N. P., Field, D., Soames. R. (2006) Anatomy and Human Movement: Structure and Function [5th Ed.], Elsevier.
- Saritha, S., Praveen Kumar, M., Supriya, G. (2012) Anatomical Variations in the Bifurcation of the Sciatic Nerve, A Cadaveric Study and its Clinical Implications , Anatomy & Physiology: Current Research, 2; 5: 1-4.
- Shiri, R., Falah-Hassani, K. (2016) The Effect of Smoking on the Risk of Sciatica: A Meta-Analysis, The American Journal of Medicine, 129: 64-73.
- Siebert, E., Prüss, H., Klingebiel, R., Failli, V., Einhäupl, K. M., Schwab. J. M. (2009) Lumbar Spinal Stenosis: Syndrome, Diagnostics and Treatment, Nature Reviews; Neurology, 5: 392-403.
- Shiri. R., Falah-Hassani. (2016) The Effect of Smoking on the Risk of Sciatica: A Meta-analysis, The American Journal of Medicine, 129; 1: 64-73.
- Toms, A. F., Rushton, L. A., Kennedy, N. R. (2017) Muscle Herniation of the Peroneus Longus Muscle Triggering Superficial Fibular Nerve Paresthesia, Sonography, 5: 1. Wiley Online Library; www.onlinelibrary.wiley.c om.
-
V , S., Adibatti , M. (2014) Study on Variant Anatomy of Sciatic Nerve,Journal of Clinical and Diagnostic Research, 8; 8: 7-9.