Nocturnal Leg Cramps (NLC)
Why Do They Occur & What Can Be Done to Help Them?
Nocturnal Leg Cramps (NLC)
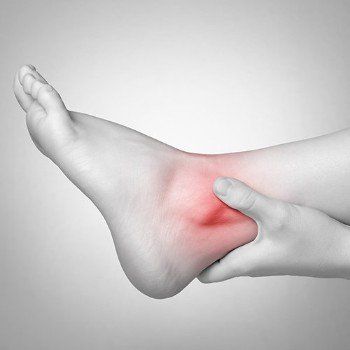
Nocturnal leg cramps (NLC) are sudden, episodic, painful and involuntary muscle contractions of either the calf, hamstrings (back of thigh) or foot and mainly occur at night (5). Up to 33% of the general population over the age of 50 have complaints related to NLC but they can occur at any age group (5, 6).
Twenty percent people who experience NLC also experience muscle cramps during the day (5). NLC are usually benign with that they do not progress to motor neuron disease (MND) or cause daytime disability (Miller and Layzer, 2005).
Medical Conditions or Pathologies Associated with NLC Include:

- Chronic liver disease
- Renal (kidney) failure (haemodialysis)
- Vascular disease
- Magnesium (Mg) or calcium (Ca2+) deficiency
- Dehydration
- Varicose veins
- Uraemia
- Diabetes
- Thyroid disease
- Hypomagnesaemia
- Hypocalcaemia (low calcium levels)
- Hypokalaemia (low potassium levels)
Investigations:

With regards to investigations, it is suggested to check electrolyte count in the urea, creatinine, potassium, magnesium and calcium concentrations, random blood glucose, and thyroid function tests. It is best to see your GP and attend to have a blood test if the problem keeps happening (1).
Medications Reported to Cause Leg Cramps Include:

- Diuretics (hypertension, liver cirrhosis, heart failure)
- Nifedepine (blood pressure and angina)
- β-agonists (asthma and heart failure)
- Steroids
- Morphine
- Cimetidine (histamine H2-receptor antagonist, stomach acid inhibitor)
- Penicillamine (anti rheumatic drug)
- Statins (lower LDL cholesterol)
- Lithium (mood stabiliser)
Cause
Muscle NLC cause is idiopathic (unknown), however, there are various hypothesis for their cause such as:
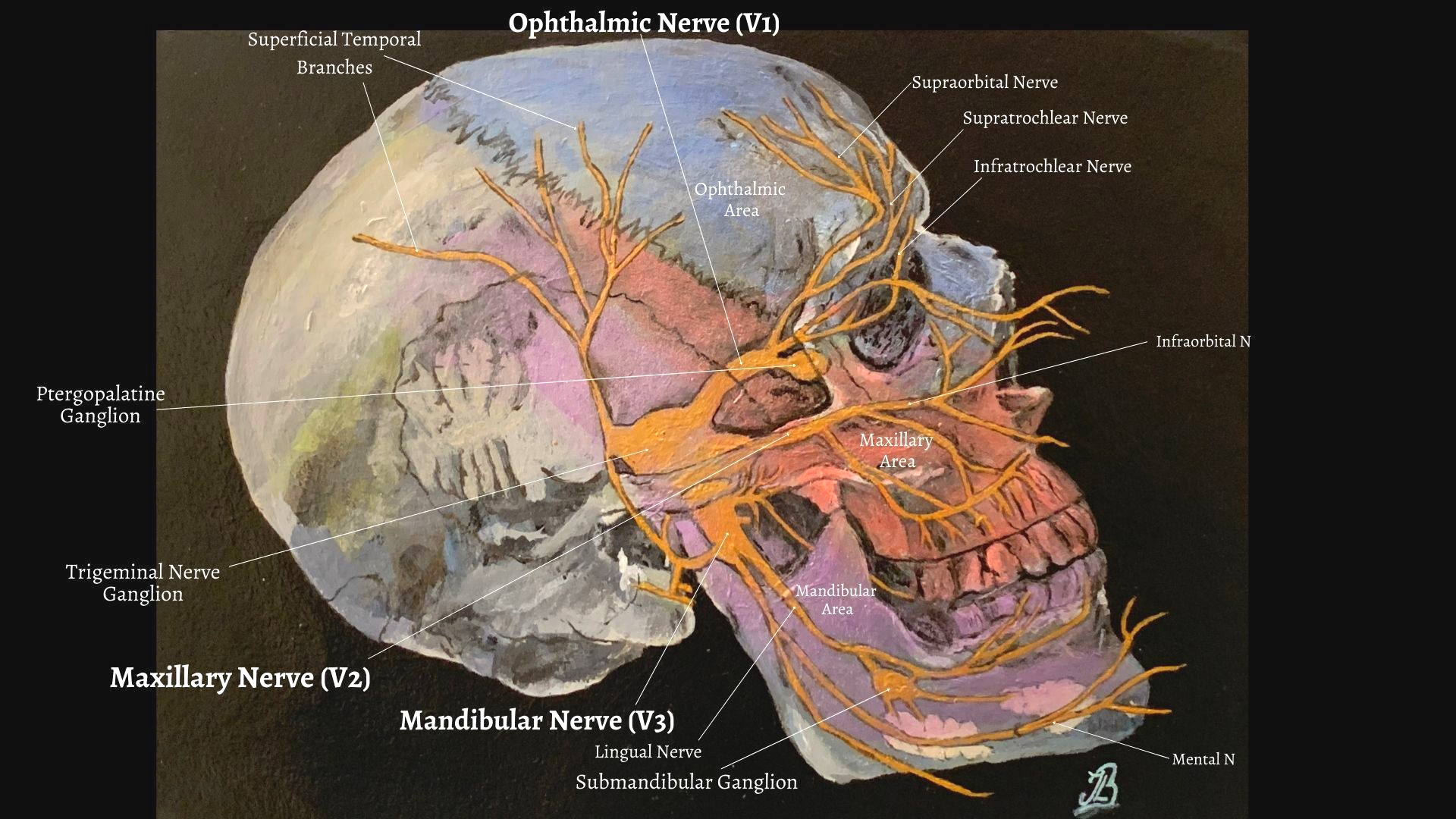
- Abnormal excitability of motor nerves
- Electrolyte imbalances.
- Dehydration.
- Accumulation of metabolites in exercised muscle.
- Use of prescriptive drugs: e.g. diuretics, steroids and morphine, quinine.
- Repetitive movements during sport or physical activity.
- Physical inactivity.
- Lack of muscle stretching leading to muscle reduced muscle and tendon length.
- Medical Conditions and pathologies; varicose veins, arthritis, hypertension, genetic disorders, endocrine and metabolic disease
What Can YOU Do To Help NLC?
Stretch & Night Time Stretching

A study by Hallegraeff et al., (2012) found that six weeks of nightly stretching of the calf and hamstring (back of the thigh) muscles reduced the frequency and intensity of nocturnal leg cramps in 80 adult participants who were over the age of 55. They concluded that stretching exercises before going to bed prevented the occurrence of nocturnal leg cramps (NLC).
Coppin et al., (2005), however, found no difference when comparing subjects who stretched at night and took quinine to manage the symptoms.
What Can WE Do To Help NLC?
Soft Tissue Massage and Instrument Assisted Soft Tissue Massage (IASTM)
Instrumental soft tissue mobilisation is the use of specific massage tools which uses deep friction massage and may benefit adhesive and contracted muscles and help heal soft tissues (7).
Deep friction massage with instrument-assisted soft tissue mobilisation (IASTM) along with other related interventions such as the Graston Technique®, ASTYM®, ASTM (Augmented Soft Tissue Mobilisation) or guasha techniques are specifically designed solid instruments that are popular in physical therapy practice, particularly for tendonitis (7).
IASTM reportedly provides strong afferent stimulation of muscles and help realign and reorganise collagen fibres in muscle, aid an increase in microcirculation and facilitate the activation of fibroblasts which is important in tendon healing (3). This technique has also been shown to disrupt rebound and cramp prone conditions (7).
References
1. Butler, J. V., Mulkerrin, E. C., O’Keefe, S. T. (2002) Nocturnal Leg Cramps In Older People, Postgrad Med J, 78: pp. 596-598.
3. Davidson, C. J., Ganion, L, R., Gehleson, G, M., Verhoestra, B., Roepke, J. E., Sevier, T. L. (1997) Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med
Sci Sports Exerc. 9: 313–319 [PubMed]
5. Hallegraeff, J. H., van der Schans, C. P., de Ruiter, R and Mathieu, H. G., and de Greef
, M. (2012)
Stretching before sleep reduces the frequency and severity of nocturnal leg cramps in older adults: a randomised trial
, Stretching for nocturnal leg cramps,
Journal of Physiotherapy, Australian Physiotherapy Association, 58: pp. 17-22.
6. Miller and Layzer (2005) Muscle Cramps, Muscle and Nerve, 32; 431-442.
7. Renzulli, J. F., Lombardo, R., Jack, Payne. (2017) Nocturnal Cramps and Introduction of a Novel Topical Therapy
Review of Pathophysiology, Etiology, and Therapeutic Approaches to Nocturnal Cramps, Internal Medicine Review; 3: 8.
8. Qiu and Kan (2017) Exercise Associated Muscle Cramps - A Current Perspective, Arch Sports Med 1(1): 3-14.